
Conversations of simulation: lessons from SESAM 2025 in Valencia
Published: 19.11.2025 / Publication / Blog
SESAM conferences have become a crucial keystone in the continuous development and conversations around simulation in healthcare. The Society for Simulation in Europe, or SESAM, is one of the biggest global societies in simulation. This year, SESAM 2025 was hosted in Valencia.
Marking the 30th annual conference, this was something of a milestone, with over 1400 attendees, almost 500 presentations, over 80 workshops and 65 countries representing (among them 69 colleagues from Ukraine). Organised at the Palacio de Congresos, this was Europe’s biggest meeting in healthcare simulation.
Simulation is constantly changing, and the words of Dr. David Gaba, the grandfather of sim (“simulation is a technique - not a technology”) [1], are as relevant today as they were over 20 years ago. This year’s theme was Developing, Adopting, and Embedding Innovative Simulation, and this was clearly visible throughout the SESAM 2025 program. Themes covered AI and VR in simulation, translational simulation for system development, interprofessional teamwork and EDI in simulation, debriefing strategies and challenges, psychological safety and emotions. Furthermore, simulation research and methodology were featured throughout: in a pre-conference writing retreat by SiReN (Simulation Research Network supported by SESAM), various methodology workshops, as well as in keynote speeches.

Some highlights from SESAM 2025
In addition to the large industry presence, wide networking and insightful sessions of the conference, worth mentioning were the keynotes. The opening speech by Prof. Carmen Gomar-Sancho from University of Barcelona took us on a journey exploring the adoption of healthcare simulation in Spain, highlighting how key organisations and societies contributed to shaping the current landscape of Spanish simulation-based practice, and how challenges of standardisation and unity remain. These are challenges we in the Finnish simulation community can clearly relate to. In her second day keynote, Vicky Tallentire from Scotland took us on an intimate journey, exploring how to inspire and support the future leaders of simulation education and scholarship; how inspiration comes from developing scholarly identities and creating the conditions to thrive (“My job is not to choose the superheroes—it’s to host the party they want to come to”). Personally, this was a powerful lesson. We need more simulation researchers in Finland.
Other keynotes were by Drs. Laurens Reinke and Uli Strauch (picture above), on DUTCH (Digital United Training Concepts for Healthcare) , a project backed by the Dutch government with €132 million and started in the Netherlands in 2022. As a grassroots collaboration, DUTCH combines healthcare professionals, knowledge institutions, and (M)EdTech partners to develop new simulation-based education along with the necessary facilities, infrastructure, and faculty to replace 50% of work-place based learning for three essential healthcare professions on a national level. Finally, the last day keynote by Dr. Linda Sonesson of King’s College London and Colonel Dr. Lazlo Fazekas of NATO Center of Excellence, showcased the large-scale simulation exercises that replicate authentic disaster environments. These exercises, particularly the NATO Vigorous Warrior series, provide high-pressure scenarios designed to enhance multiprofessional leadership, communication, and decision-making under stress. [2, 3] These are critical skills for managing major incidents and mass casualties in our concurrent times, further evidence of the power of simulation-based learning. These keynotes all highlighted not only the work that has already been done, but also the enormous potential that simulation has in our societies and communities, for tackling real-life, relevant and timely challenges.
As an associate member of the Scientific Committee, I moderated one e-Poster session and one Short Comms session. This year, unfortunately, Arcada/APSLC had no posters or research to present (next year!) but these are nevertheless wonderful opportunities to hear attendees present their work, be that development or research results. I want to highlight some work presented by our Ukrainian colleagues from Bukovinian State Medical University. Among them, Associate Professor Iryna Popova shared experiences on digital transformation in medical education in times of ongoing war, co-funded by two ERASMUS-projects, while Dr Tetiana Antofiichuk presented promising work on utilising AI and simulation to bring committed Ukrainian medical students as close to clinical reality as they can despite the war. Selected abstracts from SESAM 2025 were also published open access in Advances in Simulation (which has an updated impact factor of 4.7, amazing for a sim journal!) [4].
I co-facilitated a workshop together with our colleagues from Porto and Germany, Prof. Carla Sa Couto and Dr. Marc Lazarovici. The workshop, focused on potentials and challenges of multicentric studies, and was based on Quality.CPR, a collaboration research project by University of Porto, Ludwig-Maximillian University in Germany, and Arcada University of Applied Sciences in Finland. For more on Quality.CPR results, see: [5,6]. The workshop highlighted the high interest in taking part in multicentric projects in general, but also the need for any relevant project to be thoroughly planned, have the necessary resources and knowledge and create standards for as much as possible.
I also acted as judge in the semi-finals of SimUniversity, the annual simulation competition for undergraduate healthcare student teams. Scenarios mirror emergency situations (resuscitation, anaphylaxis, myocardial infarction). This was a great opportunity to see the high level of interprofessional work among European undergraduate healthcare students. The winning team was Portugal, but I want to highlight the team from Qatar, an all-female team of four students (medical, nursing, pharmacist, and physiotherapist!), who managed an admittedly challenging scenario involving pediatric shock and resuscitation well. This experience further emphasises the power and potential of interprofessional training. Implementing learning groups based on other characteristics than merely professions might help in changing and reshaping professional ‘identity’ perspectives [7]. As a representative of Arcada and Arcada Patient Safety and Learning Center (APSLC) and member of the EuSim Group, I participated in the traditional annual EuSim meeting. This meeting was a milestone in that, after being a network under the Region of Copenhagen and years of planning, EuSim was now founded as an independent organisation, with Arcada/APSLC as one of the founding members of this new EuSim organisation.
How should we further the conversations of simulation?
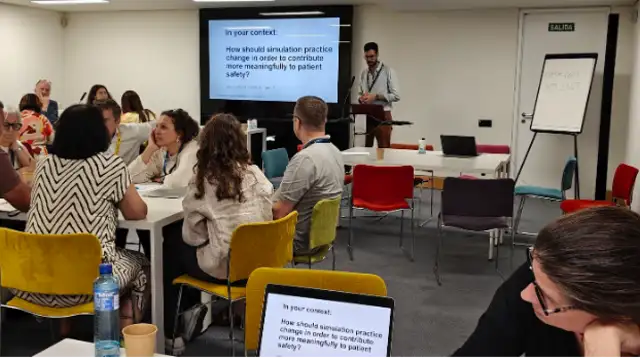
Simulation has, since its conception, been an integral part of enhancing patient safety. As highlighted by Gaba [1]; “the use of simulation to improve safety will require the full integration of its applications into the structures and routine practices of health care”. Unfortunately, in our current times, it seems ‘patient safety’ as a term and ideal has suffered a bit from inflation. We often talk the talk, but we maybe don’t really walk the walk. We know that connections between simulation and patient safety are clearly there [8]. However, we often seem to miss out on these opportunities and potential to actualise how our simulation practices could benefit patient safety. A joint workshop by WHO and SESAM, “Developing guidance for the use of Simulation to advance Patient Safety in Europe”, which allowed conference participants to engage, as focus groups, in a project on simulation practice and patient safety, made it clear that this connection needs to be strengthened, emphasised and clarified in our work as simulation educators. Instead of talking about ‘patient safety’ as a loose umbrella term, we should dig deep into what it means (i.e. medication safety, professionals wellbeing, psychologically safe teams, cognitive aids, clearer processes). Then we could focus on our simulation practices, whether they are rooted in educational or translational paradigms. [9] This would emphasise how simulation directly enhances patient safety, both for undergraduate students and professionals. We further need to use existing evidence-based simulation curriculums (instead of coming up with our own), leverage the force of local simulation societies, and, if need be, motivate simulation for patient safety through secondary measures. Maybe turning the simulation programme into a business case? [10]
AI has come to stay, and this was clear from the vast number of sessions involving AI. Although the role of generative and agentic AI in simulation has developed just within a year, the question remains how to best utilise it for simulation. SESAM 2025 went further than last year, from introducing novel AI solutions, to now thinking more about implementation and pedagogical value of AI in simulation. A workshop showcasing this was “AI-Driven Conversation Coaching for Conflict De-escalation in Healthcare”, focusing on how a combination of AI and XR technology could create scalable learning around conflict management and communication (a topic which usually requires standardized patients and less repeatability). Research into AI use in simulation has garnered interesting findings, such as by Barra et al [11], who explored the potential and risks of AI-assisted scenario design. But when it comes to simulation scenario-related use, we need to be knowledgeable of the potential risks and biases that AI may exhibit. Generative AI platforms have shown to lack gender representation [12], which might have an impact on strengthening unconscious biases in learners.
In relation to that, as simulation facilitators, we have a responsibility to address DEI (diversity, equity, and inclusivity). Simulation is the forum where we can do that, but we need to have tools to do so lest we open Pandora’s box of topics we are not, as facilitators, perhaps prepared to handle. A workshop, “JUNTOS! Together! Exploring Equity, Diversity, Intersectionality: Future Implications to Healthcare and Simulation” raised the issue of how to even define diversity (“not difference, but variety”) and how simulation could address these topics. Luckily, there are tools available to enhance reflexivity of EDI [13], and competency frameworks for faculty development [14], which we can utilise.
As I stepped off the plane at Helsinki airport, with the blasing sun and scorched streets of eastern Spain behind me, it all almost felt like stepping out of a dream state. But I realised, the power of simulation can best be tapped when we bring it out of these proverbial “bubbles” of eager simulationists, advocating simulation actively and bravely in those other contexts and communities we work in (who might not always be as open or reflective of their work as simulationists perhaps tend to be). That is when we can find opportunities for real change and new conversations around the use of simulation. I end with the words of Gaba [1]; “The simulation community must educate the public and the implementing agencies on the vision of improved patient safety using the tool of simulation.” Hoping to actively push conversations forward until we meet again at SESAM 2026 in Lyon, France. Before that, we’ll always have SESAM Annual Virtual Event (SAVE) 2026.
The author would like to thank SESAM and Worldspan for organising a fantastic conference in the wonderful city of Valencia. Participation was further made possible through external financing by Svenska Kulturfonden, whom I would also like to sincerely thank.
References
1. Gaba DM. The future vision of simulation in health care. Qual Saf Health Care. 2004 Oct;13 Suppl 1(Suppl 1):i2-10. doi: 10.1136/qhc.13.suppl_1.i2. PMID: 15465951; PMCID: PMC1765792.
2. Quinn JM, Bencko V, Bongartz AV, Stoeva P, Atanasoska Arsov A, De Porzi S, et al.. NATO and evidence-based military and disaster medicine: case for Vigorous Warrior Live Exercise Series. Cent Eur J Public Health. 2020;28(4):325-330. doi: 10.21101/cejph.a6045. PubMed PMID: 33338371.
3. Benhassine M, Quinn J, Stewart D, Arsov AA, Ianc D, Ivan M, Van Utterbeeck F. Advancing Military Medical Planning in Large Scale Combat Operations: Insights From Computer Simulation and Experimentation in NATO's Vigorous Warrior Exercise 2024. Mil Med. 2024 Aug 19;189(Suppl 3):456-464. doi: 10.1093/milmed/usae152. PMID: 39160876.
4. Selected Abstracts from the Annual Meeting of SESAM - the Society for Simulation in Europe, 2025. Adv Simul 10 (Suppl 1), 35 (2025). https://doi.org/10.1186/s41077-025-00360-4
5. Nicolau A, Bispo I, Lazarovici M, Ericsson C, Sa-Couto P, Jorge I, Vieira-Marques P, Sa-Couto C. Influence of rescuer position and arm angle on chest compression quality: An international multicentric randomized crossover simulation trial. Resusc Plus. 2024 Oct 29;20:100815. doi: 10.1016/j.resplu.2024.100815. PMID: 39526069; PMCID: PMC11550126.
6. Sa-Couto C, Sa-Couto P, Nicolau A, Lazarovici M, Ericsson C, Vieira-Marques P, Bispo I. Impact of rescuer position, arm angle, and anthropometric variables on muscle fatigue during cardiopulmonary resuscitation: an international multicentric randomized crossover simulation study. Resusc Plus. 2025 May 3;24:100971. doi: 10.1016/j.resplu.2025.100971. PMID: 40486104; PMCID: PMC12141064.
7. Neil Harrison, Susan Somerville, Prashant Kumar, Kathleen Collins. 2024. Re-Examining interprofessional simulation: Using social identity theory to explore the influence of ‘profession’ on interprofessional learning. Clinical Simulation in Nursing, Volume 97, 2024, 101652, ISSN 1876-1399, https://doi.org/10.1016/j.ecns.2024.101652.
8. Diaz-Navarro, C., Armstrong, R., Charnetski, M. et al. Global consensus statement on simulation-based practice in healthcare. Adv Simul 9, 19 (2024). https://doi.org/10.1186/s41077-024-00288-1
9. Diaz-Navarro, C., Jones, B., Pugh, G. et al. Improving quality through simulation; developing guidance to design simulation interventions following key events in healthcare. Adv Simul 9, 30 (2024). https://doi.org/10.1186/s41077-024-00300-8
10. Szabo, R.A., Molloy, E., Allen, K.J. et al. Leaders’ experiences of embedding a simulation-based education programme in a teaching hospital: an interview study informed by normalisation process theory. Adv Simul 9, 21 (2024). https://doi.org/10.1186/s41077-024-00294-3
11. Barra, F.L., Rodella, G., Costa, A. et al. From prompt to platform: an agentic AI workflow for healthcare simulation scenario design. Adv Simul 10, 29 (2025). https://doi.org/10.1186/s41077-025-00357-z
12. Berger-Estilita, J., Gisselbaek, M., Devos, A. et al. AI and inclusion in simulation education and leadership: a global cross-sectional evaluation of diversity. Adv Simul 10, 26 (2025). https://doi.org/10.1186/s41077-025-00355-1
13. Purdy, E., Symon, B., Marks, RE. et al. Exploring equity, diversity, and inclusion in a simulation program using the SIM-EDI tool: the impact of a reflexive tool for simulation educators. Adv Simul 8, 11 (2023). https://doi.org/10.1186/s41077-023-00250-7
14. Mutch, J., Golden, S., Purdy, E. et al. Equity, diversity and inclusion in simulation-based education: constructing a developmental framework for medical educators. Adv Simul 9, 20 (2024). https://doi.org/10.1186/s41077-024-0029…